Design
A retrospective analysis.
Time and setting
The experiment was conducted in the Joint Surgery of Affiliated Hospital of Qingdao University in China from February 2013 to February 2014.
Subjects
All patients with osteoarthritis undergoing primary bilateral TKA were recruited in this study. The indication was degenerative osteoarthritis that was severe enough to warrant TKA after a nonoperative therapy. The study has been approved by the Clinical Research Ethics Committee of the Affiliated Hospital of Qingdao University in China.
Inclusion criteria
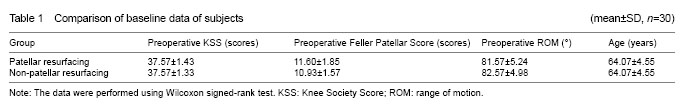
(1) Those consistent with the diagnostic criteria of osteoarthritis developed by American College of Rheumatology; (2) those undergoing one-stage bilateral TKA, with one side of knee for patellar resurfacing and the other not; (3) all patients were operated by the same surgeon team; (4) those followed up for more than 1 year postoperatively; and (5) those receiving the Stryker Scopio NRG CR total knee prosthesis (Stryker Orthopedics, Mahwah, NJ, USA). As a result, 30 cases (60 knees; 7 males, 23 females; a mean age of 64.07±4.55 years (57-75 years) were included in our study.
Exclusion criteria
A history of patellar fracture, patellectomy, high tibial or distal femoral osteotomy, any operation involving the extensor mechanism, septic arthritis of the knee or osteomyelitis, severe deformity (varus angulation, valgus angulation, or flexion contracture of more than 15°), and severe medical disability that limited the ability to walk.
Implantation
The prosthesis of all patients was Scorpio NRG total knee arthroplasty system, which purchased from America Stryker Company.
Methods
Surgical methods
All patients were operated by the same surgeon team that had rich experience of TKA. Under epidural/general anesthesia, the patient was treated by a median incision of anterior knee for medial parapatellar approach. After resection of hyperplastic synovial membrane, medial and lateral menisci, anterior and posterior cruciate ligaments and part of infrapatellar fat pad, a valgus distal femoral osteotomy was performed with the entry point 1 cm before the attachment site of posterior cruciate ligament and the valgus angle of about 6 degrees. A proximal tibial osteotomy was also performed to install ankle fixator, with the tip of which pointing at the interdigital gap between the first and second toes. Then a medial osteotomy with opening wedge of 2 mm and a lateral osteotomy of 10 mm were performed to release the soft tissues such as knee joint capsule and collateral ligaments and to balance the extension and flexion forces of the knee. A knee joint testing mold of appropriate size was used to determine the patellar thickness so that the substitute to be installed had the same or smaller (not than 2 mm) thickness. After determining the size of patellar mold, an osteotomy was then performed on the patellar surface to fix the mold. All prostheses were installed with bone cement. Non-patellar resurfacing group: After removing the proliferated patellar bone masses, the margins of patella were smoothened and the patella was placed on its original anatomical site. The retinacula of patella were electrically released to recover the normal trajectory of patella, with special attentions paid to protect the blood supply of the patella. All cases received parapatellar denervation. In general, a drainage tube was placed in the articular cavity. During the surgery, the patient’s blood loss and surgical time were recorded, and after the surgery, the whole affected limb was compressively dressed by elastic bandages.
Postoperative treatments and rehabilitation training
The drainage tube was removed 48 hours after the surgery. Routine antibiotics were administered for 5 to 7 days. Anticoagulant drugs were also given and the affected limb was elevated to prevent deep venous thrombosis. Other treatments were used for detumescence, stop bleeding and pain relief. In general, the sutures were removed 3 weeks after the surgery.
The patient began functional exercise on day 1 following surgery, mainly including active isometric contraction of quadriceps femoris and ankle joint extension and flexion. After removing drainage tube, the patient was encouraged to lift up his/her leg and the knee joint was passively extended or flexed. The range of motion (ROM) of knee joint was gradually increased from 30 degrees during the training that lasted for 0.5-1.0 hours per time and 4 times per day. In general, on day 7 after the patient’s discharge, the ROM reached about 0-120 degrees. The patient was informed of continuing functional training after the discharge.
Main outcome measures
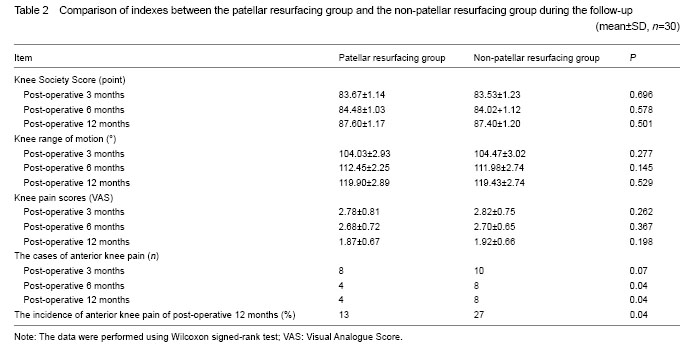
Anterioposterior and lateral radiography of bilateral knees was ordered during the reexamination at 3 months following the surgery, after which the patient was reexamined every 3 months during the 1-year follow-up. For every follow-up, the recorded indexes included: symptomatic relief (such as pain), life satisfaction, living ability, walking distance, gait, the ability of walking upstairs and downstairs, muscle strength, deformed conditions, maximum range of knee flexion, and ROM of knee. In the meantime, the patient was also evaluated according to Knee Society Score (KSS), Feller Patellar Score and Anterior Knee Pain Scale. All complications occurring during the follow-up period such as anterior knee pain, patellar fracture, osteonecrosis of the patella, patellar instability, patellar ligament rupture, patellar clunk, prosthesis failure and patellar prosthetic revision were carefully recorded.
Statistical analysis
All data were performed using the SPSS version 21.0.1 statistical package. Categorical data were compared using the chi-square test. Non-parametric statistics were used for analysis of continuous variables when data did not meet the assumptions of parametric tests. A paired samples t-test or the Wilcoxon signed-rank test was used to analyze score differences between the two groups.
Logistic regression analysis was used to assess associations between potential explanatory variables and the categorical, independent variable post-operative anterior knee pain. Residual analysis was performed and confirmed the validity of these models. For the main outcomes after operation, the significance level was set at P ≤ 0.05. Power analysis determined that a sample size of 60 gave a power of 92% to detect a ten-point difference in the mean change in the knee pain score between groups, which represented one half of an SD in change scores obtained from a pilot study of TKA patients. Since the study was one of equivalence, a confidence interval for the change score which fell within a point range of -10 to +10 was statistically significant evidence for equivalence. The Statistical Package for Social Sciences version 21.0 was used for data processing. Measurement data were shown in mean ± SD. Between-group comparison was performed with paired samples t-test and the incidence rates of postoperative anterior patellar pain were compared using paired chi-square test, with the statistical difference defined as P < 0.05.